Emotional Storm: Understanding Chronic Illness Impact
Explore the impact of chronic illness on emotional health and discover effective coping strategies for better well-being.

Chronic Illness and Emotional Health
Impact of Chronic Illness
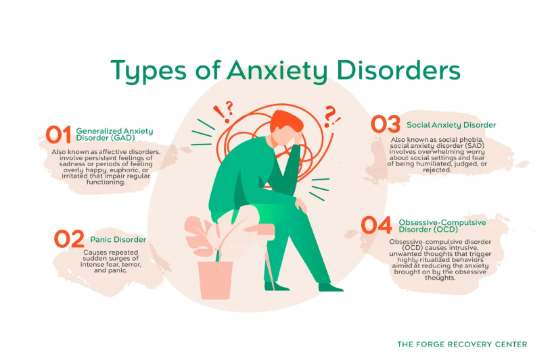
Chronic illnesses can significantly affect an individual's emotional health. Research indicates that people with chronic diseases are at a higher risk of developing depression and other mood disorders. The symptoms of chronic conditions, such as pain, fatigue, and invisible struggles, can create an environment conducive to stress and anxiety. Adjustments in lifestyle and aspirations are common, and many individuals may experience grief over their circumstances before adapting. This adaptation can lead to chronic distress, resulting in psychiatric disorders, primarily depression or anxiety.
The prevalence of mood disorders in those with chronic conditions is notably higher compared to the general population. For instance, rates of affective disorders in individuals with conditions like diabetes or rheumatoid arthritis can range from 20% to 25%, which is significantly above the community's typical depression rate of approximately 4% to 8%.
Chronic ConditionAffective Disorder Rates (%)Diabetes20 - 25Rheumatoid Arthritis20 - 25General Population4 - 8

Interconnection Between Chronic Disease and Mental Health
The relationship between chronic illness and mental health is reciprocal. Individuals with chronic diseases not only face an increased risk of developing mood disorders, but those with existing depression also face a greater chance of developing chronic conditions. Research shows that depression can heighten the likelihood of serious health issues, including heart disease, diabetes, stroke, osteoporosis, and Alzheimer’s disease [3].
Understanding this interconnection is essential for creating effective management strategies for those dealing with chronic conditions and mood disorders. As mental health impacts coping mechanisms regarding physical health, individuals may struggle to manage their chronic conditions effectively when also battling emotional challenges. Ensuring emotional well-being is therefore crucial for overall health and quality of life.
For more insights on mental health, explore information on emotional regulation techniques or the impact of diet on emotional well-being. Additionally, consider strategies for preventing emotional burnout in the context of chronic illness.
Signs and Symptoms of Depression
Identifying depression is crucial, especially when it coexists with chronic illness. Understanding the signs and symptoms can help in recognizing whether one may need to seek support or treatment.
Recognizing Depression
Depression is one of the most prevalent complications associated with chronic illness, impacting up to one-third of individuals with serious medical conditions. Common indicators of depression include:
Sign/SymptomDescriptionPersistent SadnessOngoing feelings of emptiness or sadness.HopelessnessA sense of despair or a lack of hope about the future.Lack of InterestNo longer enjoying hobbies or activities that were once pleasurable.FatigueConstant tiredness or low energy levels.IrritabilityIncreased frustration or mood swings.
Understanding the Symptoms
The symptoms of depression can often overlap with the physical manifestations of chronic illnesses. This makes it challenging to diagnose accurately. Symptoms to be aware of include:
Individuals with chronic conditions may experience these symptoms differently, and risk factors such as a history of depression, social isolation, and lack of emotional support can heighten the likelihood of developing depression [2].
The impact of chronic illness on emotional health is profound, often leading to a vicious cycle where depression exacerbates the illness. Poor mental health can worsen physical outcomes, increase disability, and raise the risk of mortality. Understanding these signs is essential for timely intervention, which can include exploring emotional regulation techniques or seeking support through therapy. Recognizing and addressing these symptoms can facilitate a better quality of life for those affected.
Managing Depression with Chronic Illness
Addressing the impact of chronic illness on emotional health involves understanding effective treatment options and fostering a collaborative care approach.
Treatment Options
There are several treatment methods available for managing depression, especially for individuals facing the challenges of chronic conditions. Options include psychotherapy, medication, or a combination of both. If an individual cannot or does not wish to take antidepressant medication, alternative evidence-based treatments are also available [3].
Here’s a table summarizing common treatment options for depression:
Treatment MethodDescriptionPsychotherapyTalk therapy to help explore feelings and coping strategiesMedicationAntidepressants prescribed based on individual needsEvidence-based therapiesAlternatives such as cognitive behavioral therapy or mindfulness practices (role of mindfulness in emotional stability)Lifestyle modificationsStrategies including exercise as a tool for mood enhancement (exercise as a tool for mood enhancement) and dietary changes (impact of diet on emotional well-being)
Research indicates that early diagnosis and treatment of depression in individuals with chronic conditions can lead to improvement in their overall medical condition, quality of life, and treatment adherence [4].
Collaborative Care Approach
A collaborative care model is beneficial for those managing both chronic illness and depression. This approach involves a team that may include healthcare providers, mental health professionals, and support from family or friends. The interconnection of physical and mental health means that both should be addressed simultaneously for the best outcomes.
The collaborative care model encourages open communication among all parties involved in the individual’s health journey. This model also allows for the development of personalized treatment plans that cater to the unique needs of the individual, leading to better management of mood disorders and chronic illnesses [1].
Incorporating the support of family members can further reduce feelings of isolation and frustration experienced by those with chronic illnesses. Support systems can help maintain emotional stability and provide encouragement in implementing emotional regulation techniques as part of their coping strategies.
By focusing on both the treatment options available and the collaborative care model, individuals can better manage the impact of chronic illness on their emotional health, improving their overall well-being and quality of life. For those seeking additional resources, exploring strategies for preventing emotional burnout (strategies for preventing emotional burnout) can be valuable.
Challenges of Chronic Illness
Chronic illnesses pose numerous challenges that significantly affect an individual's emotional health. The impact of chronic illness on emotional well-being can be profound, influencing daily life and interpersonal relationships.
Effects on Daily Life
Living with a chronic illness often entails coping with invisible symptoms like pain, fatigue, and mood disorders. These symptoms can hinder daily activities, making it difficult for individuals to maintain their usual routines. For many, chronic conditions lead to stress, anxiety, and depression, complicating their ability to manage daily tasks [1].
The table below illustrates common daily life challenges faced by individuals with chronic illness:
Daily Life AspectPotential ChallengesMobilityLimited ability to move freelySocial ActivitiesWithdrawal from social interactionsSelf-CareDifficulty in performing personal careEmotional RegulationIncreased anxiety and mood swingsRoutine ManagementTrouble keeping up with daily tasks
Physical changes due to chronic illness can also lead to a negative self-image, further exacerbating emotional challenges. Individuals might experience social withdrawal, which can contribute to developing mood disorders like depression and anxiety.
Impact on Work and Relationships
Chronic illnesses can considerably influence an individual's professional life. Many must adjust work routines due to their health condition, which can result in financial difficulties and longer times to complete tasks. This may create a need for additional help from colleagues or family members [1].
The emotional impact extends to relationships as well. Family members may experience frustration, anger, hopelessness, and depression due to the challenges posed by a loved one's chronic condition. The uncertainty about the future can create stress and feelings of loss of control for both the individual and their loved ones.
Chronic illness requires adjustments not just for the person affected, but also for those they are close to. Awareness of these impacts is crucial for developing supportive coping strategies and ensuring the emotional health of all involved.
For more insights into how chronic illness affects emotional health, consider exploring topics on the impact of mood disorders on academic performance and emotional regulation techniques.
Seeking Support and Coping Strategies
Addressing the emotional challenges that arise from chronic illness is crucial for overall well-being. This section examines the importance of emotional support and the development of personalized treatment plans for managing the impact of chronic illness on emotional health.
Importance of Emotional Support
Emotional support plays a critical role in achieving person-centered care for individuals dealing with chronic conditions. Patients across various healthcare settings highly value emotional support as it fosters a sense of warmth, safety, and humanity [5]. This support can come from various sources, including friends, family, support groups, and healthcare providers.
Research indicates that when patients feel listened to and validated during their interactions with clinicians, it enhances their engagement in treatment and builds trust. Mindful listening helps patients express their feelings and concerns, which contributes to their emotional stability.
Source of SupportBenefitsFriends and FamilyEmotional comfort and understandingSupport GroupsShared experiences and coping strategiesHealthcare ProvidersProfessional guidance and personalized care
Establishing a strong support system can alleviate feelings of isolation and empower individuals to cope more effectively with their emotional burdens.
Developing Personalized Treatment Plans
Creating personalized treatment plans is essential for addressing the unique emotional health needs of individuals with chronic illnesses. These plans should take into account the specific challenges faced by patients, as well as their preferences and goals.
Components of a personalized treatment plan can include:
Collaborative goal-setting is also important. This ensures that the treatment plan aligns with the individual's values and desired outcomes, leading to more effective management of the emotional effects of chronic illness. For those seeking additional strategies, exploring topics such as strategies for preventing emotional burnout and supporting a loved one with mood challenges can provide further insights.
Addressing Mental Health Concerns
Diagnosis and Treatment
Diagnosing depression in individuals with chronic conditions can be complex. Symptoms such as disturbed sleep, impaired appetite, and lack of energy may overlap with those of the medical condition or its treatment. Clinicians must be vigilant, as even mild depression can lead to reduced motivation in accessing medical care and adhering to treatment plans. For instance, research indicates that depression adversely affects patients' coping mechanisms regarding pain and can compromise relationships, potentially leading to severe outcomes, including suicide [2].
To ensure an accurate diagnosis, healthcare providers should consider the risk factors for depression, including a history of depression, major functional disability, persistent pain, adverse social circumstances, and inadequate emotional support. A structured approach to assess these factors can guide effective treatment strategies for patients.
Risk FactorDescriptionHistory of DepressionPrevious episodes of depression increase current risk.Major Functional DisabilityLimitations in day-to-day activities correlate with emotional issues.Persistent PainChronic pain can exacerbate feelings of hopelessness.Adverse Social CircumstancesStrained relationships or lack of support can negatively affect mental health.Inadequate Emotional SupportAbsence of a supportive network can lead to isolation and despair.
Impact of Emotional Support
Emotional support plays a vital role in the recovery and management of mood disorders in patients with chronic illnesses. Studies indicate that patients value a warm, personal environment where they feel treated as human beings. This compassionate interaction often enhances the therapeutic relationship, fostering trust and openness during recovery phases [5]. Clinicians who demonstrate genuine emotional concern and empathy significantly impact patient outcomes, particularly when engaging with patients during rehabilitation.
Moreover, individuals receiving emotional support report reduced feelings of anxiety, lower levels of depression, and improved coping mechanisms. Encouraging open communication between patients and healthcare providers can also facilitate better treatment adherence, contributing to improved physical and mental health outcomes overall.
To further support emotional well-being, patients may benefit from various coping strategies and treatment approaches. For insights on enhancing mood, explore topics such as the impact of diet on emotional well-being, exercise as a tool for mood enhancement, and emotional regulation techniques. Integrating these strategies can help bolster mental health alongside medical management, leading to a more holistic approach to chronic illness care.
References
[2]:
[3]:
[4]:
[5]:
[6]:
[7]:
More Resources
A team ready to start your journey.
Get in touch — today.
We are a safe space – a haven for exceptional individuals to receive discreet, personalized, in-person treatment and care.
.avif)