Effective Management of Rapid Cycling in Bipolar Disorder
Explore rapid cycling in bipolar disorder: causes and management strategies for better emotional balance.

Understanding Rapid Cycling in Bipolar Disorder
Definition and Frequency
Rapid cycling in bipolar disorder refers to the occurrence of four or more distinct mood episodes within a 12-month period. These episodes can be manic, hypomanic, or depressive. Studies indicate that between 10% to 20% of individuals diagnosed with bipolar disorder experience rapid cycling. Notably, women are more likely to be affected, with approximately 70% to 90% of rapid cycling cases occurring in females.
The prevalence of rapid cycling is relatively low in the general population. However, within the community of those diagnosed with bipolar disorder, it is significantly more common, with research showing about a third of individuals with a lifetime diagnosis of bipolar disorder and 40% of those experiencing symptoms within the past year classified as rapid cycling.
StatisticPercentageIndividuals with bipolar disorder10% - 20%Women affected by rapid cycling70% - 90%Lifetime bipolar disorder with rapid cycling~33%12-month bipolar disorder with rapid cycling~40%

Impact on Individuals
Rapid cycling can have profound effects on an individual's life. Those experiencing this condition often face greater episode frequency, which can lead to heightened severity of symptoms and increased impairment in daily functioning when compared to individuals with non-rapid cycling bipolar disorder. This rapid fluctuation between mood states can disrupt personal relationships, work, and overall quality of life.
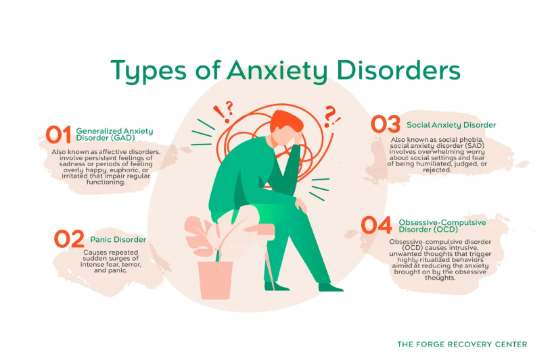
Individuals may also encounter a complex interplay with other mental health disorders, resulting in a higher likelihood of comorbidity. For instance, anxiety disorders and substance use issues can commonly arise alongside rapid cycling bipolar disorder.
Additionally, there are challenges in managing this type of bipolar disorder, as standard treatment approaches may not be as effective. Research indicates that nearly 69% of patients with medication-resistant symptoms reported positive responses to Electroconvulsive therapy (ECT) as a treatment option. Understanding rapid cycling in bipolar disorder: causes and management is essential for supporting individuals and developing effective treatment strategies.
For more information on mood disorders, refer to our article on the spectrum of mood disorders explained.
Factors Contributing to Rapid Cycling
Understanding the factors that contribute to rapid cycling in bipolar disorder is crucial for effective treatment and management. Two significant areas of focus are gender disparities and potential triggers and causes.
Gender Disparities
Research indicates that women are more likely to experience rapid cycling in bipolar disorder compared to men. About 70-90% of individuals with rapid cycling are women. It is estimated that 10-20% of those diagnosed with bipolar disorder will encounter rapid cycling. The reasons for this discrepancy can be complex and may relate to hormonal differences, life stressors, and societal factors that are more prevalent among women.
A major depressive episode is often a part of the rapid cycling experience, typically lasting around two weeks. Symptoms may include experiencing five or more depressive symptoms from a defined list. Awareness of these gender differences is essential for targeted interventions and support systems. For further insights, one can refer to our article on bipolar disorder: navigating the highs and lows.
Potential Triggers and Causes
Several potential triggers and causes are linked to rapid cycling in bipolar disorder:
Understanding these factors can help guide treatment choices and potentially mitigate the impact of rapid cycling on individuals. For a broader perspective on mood disorders, consider exploring our article on the spectrum of mood disorders explained.
Manifestations of Rapid Cycling
Types of Mood Episodes
Individuals with rapid cycling bipolar disorder experience a distinct pattern of mood episodes throughout their lives. These episodes can be categorized as manic, hypomanic, depressive, or mixed states.
Mood Episode TypeDescriptionManic EpisodeCharacterized by elevated mood, increased activity, and often reckless behavior. Symptoms may include excessive energy, decreased need for sleep, and racing thoughts.Hypomanic EpisodeSimilar to mania but less severe. Individuals may feel unusually energetic and productive but do not experience significant impairment.Depressive EpisodeInvolves feelings of sadness, hopelessness, and a loss of interest in activities. These episodes can lead to significant functional impairment.Mixed EpisodeSymptoms of both manic and depressive states occur simultaneously, resulting in a complex emotional experience.
It is important to recognize that the rapid cycling course can significantly affect treatment strategies. Mood stabilizers and sometimes antipsychotic medications are essential in managing these varying states.
Mixed States and Symptomatology
Mixed states are a unique aspect of rapid cycling bipolar disorder, presenting both manic and depressive symptoms at the same time. During these episodes, individuals may feel energized yet despondent, leading to experiences that are both exhilarating and distressing. They might describe feeling "revved up" while simultaneously grappling with anguish and despair [1]. This combination can make diagnosing and treating individuals particularly challenging.
The symptomatology of mixed states includes:
Individuals experiencing mixed episodes may be at an increased risk for negative outcomes, including suicidal behavior. Research indicates that 8% to 20% of people with bipolar disorder may die by suicide, with those experiencing rapid cycling being at even greater risk. Addressing these symptoms promptly and effectively is crucial in managing overall well-being and maintaining functionality.
For more details on management strategies for rapid cycling in bipolar disorder, consider exploring additional resources like mood stabilizers: types effectiveness and side effects and psychotherapy approaches for mood disorders.
Diagnosis and Assessment
Criteria for Rapid Cycling
Rapid cycling in bipolar disorder is characterized by a specific pattern of mood episodes. To meet the criteria for rapid cycling, an individual must experience four or more episodes of mania, hypomania, or depressive episodes within a 12-month period. This pattern can occur in any type of bipolar disorder and may be temporary for some individuals [4].
To clarify the criteria for rapid cycling, the following table outlines the relationship between the number of episodes and the classification of rapid cycling.
EpisodesClassification0-3Non-rapid cycling bipolar disorder4 or moreRapid cycling bipolar disorder
It's important to recognize that rapid cycling can worsen the primary disorder and may indicate greater symptom severity and impairment compared to non-rapid cycling varieties [2]. Early detection and diagnosis of rapid cycling can improve treatment strategies and enhance long-term outcomes.
Differential Diagnosis Challenges
Differential diagnosis for rapid cycling can present several challenges. Distinguishing rapid cycling from other types of mood disorders, such as mixed episodes in mood disorders: when depression and mania coexist or cyclothymic disorder: when mood swings are milder but persistent, requires careful assessment. Mixed episodes present symptoms of both mania and depression simultaneously, which may complicate the identification of rapid cycling.
Additionally, the prevalence of rapid cycling is relatively low, with a 12-month prevalence of only 0.3% [2]. This rarity can lead to misdiagnosis or delayed recognition. Factors such as age of onset, comorbidity with anxiety disorders, and the severity of depressive symptoms may also influence the diagnostic process. Many individuals with rapid cycling also report greater impairment and a higher use of health services.
Overall, the nuanced nature of rapid cycling necessitates a thorough exploration of an individual’s mood history and symptom patterns, ensuring appropriate diagnosis and management in the context of mood disorders.
Treatment Approaches for Rapid Cycling
The management of rapid cycling in bipolar disorder typically involves a combination of medication and therapy strategies tailored to individual needs. Understanding these approaches is crucial for effective treatment.
Medication Options
Effective pharmacotherapy is a key component in managing rapid cycling. Various medications can be utilized depending on the nature of mood episodes experienced.
MedicationIndicationAripiprazoleAcute manic or mixed episodes, relapse prevention (PubMed)OlanzapineAcute manic or mixed episodesValproateAcute manic or mixed episodesQuetiapineAcute depressive episodesLamotrigineRelapse prevention
It's important to note that the use of antidepressants can sometimes lead to increased risks of rapid cycling in bipolar disorder. For example, studies suggest that during depressive episodes, antidepressants may worsen the rapid-cycling course. Thus, careful consideration must be given to treatment plans.
Therapy and Management Strategies
Psychotherapy also plays a crucial role in the management of rapid cycling. Cognitive behavioral therapy (CBT) has been shown to significantly reduce relapse rates in individuals with bipolar I and II disorders. Other therapeutic approaches that can be beneficial include interpersonal and social rhythm therapy, which focuses on stabilizing daily routines and rhythms [3].
In addition to therapy, maintaining good sleep hygiene is vital. Individuals experiencing rapid cycling may find benefits in consistent circadian rhythms, which can help stabilize mood fluctuations.
Overall, a comprehensive treatment plan that incorporates both medication and psychotherapy is essential for managing rapid cycling effectively in bipolar disorder. For further information on related mood disorders, readers can explore topics such as understanding mood disorders: an overview and bipolar disorder: navigating the highs and lows.
Managing Challenges and Risks
Suicide Risk and Prevention
Individuals diagnosed with bipolar disorder, particularly those exhibiting rapid cycling, face a significantly higher risk of suicide. Research indicates that people with bipolar disorder are 10 to 20 times more likely to attempt suicide compared to the general population. This risk is heightened in those with rapid cycling, as they often experience more challenging symptoms and greater difficulty in long-term management. Frequent hospitalizations are common in this demographic, showcasing the urgency of intervention. Long-term use of lithium has been shown to effectively reduce the risk of suicide in these individuals [7].
To mitigate this risk, mental health professionals should regularly assess suicidal thoughts and behaviors in individuals with rapid cycling bipolar disorder. Here are some key strategies for suicide prevention:
StrategyDescriptionRegular TherapyOngoing psychotherapy can provide support and coping strategies.Medication ManagementConsistent medication adherence, including mood stabilizers, can help manage mood fluctuations.Crisis PlanningDeveloping a crisis plan with professionals can prepare individuals for potential emergencies.Support NetworksEncouraging connections with family and friends can provide emotional support.
Substance Abuse Concerns
Substance abuse is another significant concern for individuals with bipolar disorder. Approximately 60% of individuals with this diagnosis abuse drugs or alcohol, which complicates their mental health condition and treatment efficacy. Substance use can lead to more severe symptoms, increased mood instability, and a greater likelihood of rapid cycling episodes.
It is essential for treatment plans to address substance abuse alongside bipolar disorder management. Here are some considerations for managing substance use:
ApproachDescriptionComprehensive AssessmentEvaluate both bipolar disorder and substance abuse to devise a cohesive treatment plan.Dual Diagnosis TreatmentOffer integrated interventions that address both conditions simultaneously.EducationProvide information on the risks associated with substance use and mood disorders.Support GroupsEncourage participation in support groups for individuals facing both bipolar disorder and substance use challenges.
By recognizing and addressing the risks associated with suicide and substance abuse, individuals with rapid cycling in bipolar disorder can better manage their condition and improve their overall quality of life. For more information on mood disorders, refer to our overview on understanding mood disorders: an overview and the spectrum of mood disorders explained.
References
[2]:
[3]:
[4]:
[5]:
[6]:
[7]:
More Resources
A team ready to start your journey.
Get in touch — today.
We are a safe space – a haven for exceptional individuals to receive discreet, personalized, in-person treatment and care.
.avif)